
Faculty from the Duke Clinical Research Institute (DCRI) shared new research and offered expert perspectives on emerging issues and advancements in cardiovascular care as part of more than 45 sessions during the American College of Cardiology (ACC) Scientific Sessions, held March 29-31 in Chicago.
This year’s ACC annual meeting highlighted innovation as a cornerstone of progress and received 17% more submissions than in years past, with more than 9,000 submissions total.
DCRI faculty participated as presenters, moderators for main-stage sessions, panelists during fireside chats and town hall-style discussions, debate hosts, and contestants in friendly competitions during the three-day meeting.
March 29 Sessions
RESILIENCE Insights on Research Consent, Recruitment Strategies
Health systems vary widely in how they approach research consent and recruitment strategies, according to two analyses presented by DCRI fellow Pishoy Gouda, MB, BCH, BAO, MSC, during a moderated ACC poster session.
Gouda and his colleagues examined various informed consent approaches within the RESILIENCE study, comparing traditional text-only consent forms with three audiovisual alternatives: forms that included physician videos, patient videos, or animations.

The results demonstrated no significant differences in consent rates between the four modalities, which ranged from 53% to 62.4% across groups. Additionally, patient comprehension of consent information, measured by a seven-question quiz, remained constant regardless of approach, with approximately 86.4% of participants demonstrating an adequate understanding of the information shared with them.
The second analysis focused on recruitment strategies, utilizing a two-by-two factorial design to compare two contact methods (email versus patient portal) and two types of message content (altruistic versus individualistic appeals). The findings indicated that email messages generated significantly higher engagement rates than communications sent via the patient portal (9.9% compared to 5.9%). While there was no overall difference in effectiveness based on message content, participants under the age of 60 responded more positively to altruistic messaging.
"We really need to improve the efficiency of the entire research enterprise to understand the motivations of a spectrum of potential participants," Gouda said. "We then need to harness evidence-based strategies to reach patients and increase their willingness to participate in research."
The findings highlight important considerations for clinical researchers, as approximately 80% of randomized controlled trials fail to meet their enrollment targets. Despite improved digital communication options, participant recruitment and retention continue to face significant challenges.
Gouda suggested future research should investigate more interactive consent processes and explore innovative recruitment strategies tailored to different demographic groups, potentially taking cues from industry marketing techniques.
The RESILIENCE study (NCT04551872) examines factors contributing to cardiovascular disease resistance and resilience among individuals with obesity.
Advocating for Ongoing AI Monitoring in Healthcare Systems
DCRI's Robert Califf, MD, emphasized the need for continuous monitoring of artificial intelligence (AI) systems in healthcare during an ACC intensive session on regulatory and legal considerations in clinical AI implementation.
Califf compared AI oversight to monitoring an intensive care unit patient, noting that both require vigilant attention as conditions can change rapidly.

"This post-market monitoring, in my opinion, is the most important thing that we need to figure out because, as best I can tell, there's not a single health system in the U.S. today that's capable of actually doing a good job of monitoring deployed AI," he said.
The former commissioner of the FDA, who now serves as an instructor of medicine at the Duke University School of Medicine, advocated for a balanced approach to AI regulation that leverages technological potential while still protecting patients from potential harms.
Califf identified several opportunities with the increasingly utilized technology, including reduced administrative burden, immediate access to universal knowledge, improved diagnostics, and enhanced medical devices. However, he also highlighted the significant risks, such as algorithmic bias, propagation of inaccurate information, AI hallucinations, and algorithms that degrade over time.
Perhaps most concerning, Califf noted, is the misalignment between financial incentives and patient outcomes.
"When you deploy an AI system in a living environment, things change," he explained. "AI algorithms are totally dependent on the input and the direction that's taken in terms of the output that's desired."
Traditional regulatory frameworks won't work for rapidly evolving AI technologies, Califf emphasized, drawing parallels to the food industry where producers follow established principles between infrequent inspections. Instead, he proposed a "living ecosystem" approach with continuous validation in specific usage contexts.
"Every element of the system is trying to operate on some financial well-being, leading to a lot of hoarding and difficulty with information," Califf said. "I hope that AI will be a motivating force to pull the information ecosystem together, with the primary focus being the outcomes of patients, not primarily the financial well-being of the institution."
He closed out his presentation by recommending standardized "AI algorithm cards" for transparency, establishing clear liability frameworks to address the challenges ahead, and implementing local, recurrent validation processes.
When Pressure Does Not Equal Volume: Exploring Cases of Hypervolemia Despite Normal Pressures
During a Saturday afternoon session, DCRI’s Marat Fudim, MD, MHS, challenged the conventional paradigm that pressure serves as a surrogate for volume in hemodynamic assessments, exploring cases of hypervolemia despite normal pressures.
Hypervolemia refers to a medical condition characterized by having too much fluid in the body. Fudim emphasized that decongestion is not solely about diuresis, (an excess production of urine), noting that 28% of patients gain weight during hospitalization. This underscores the complexity of managing heart failure, where most of the water resides inside cells, with only a small proportion in the intravascular space.
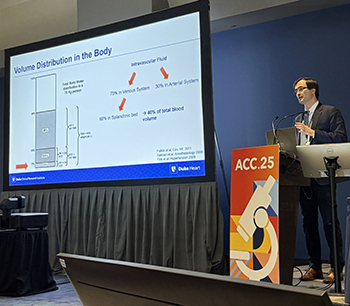
Fudim highlighted discrepancies in assessing congestion among heart failure patients. He pointed out that attending physicians, equipped with catheterization data, often fail to accurately predict pressures, with attending physicians or fellows being wrong around half of the time. The discrepancy was further illustrated by data showing that 20% of patients gain weight during hospitalization despite the use of diuretics.
Fudim shared an experiment in which patients hospitalized with heart failure with reduced ejection fraction (HFrEF) who had their diuretic and guideline-directed medical therapy medications withdrawn showed increased symptoms and pressure without significant weight gain. This finding challenges the notion that volume retention is necessary for cardiac decompensation.
The session also explored the distribution of water in the human body, with 60% residing intracellularly and only 5% in the intravascular space. Fudim explained that drugs targeting the intravascular system, such as diuretics, affect a small proportion of body water.
Fudim’s session emphasized the importance of understanding the complex relationship between intra- and extravascular spaces for better heart failure management.
"Pressure does not equal volume, and the relationship compression bond can be disconnected,” Fudim said. “We've got to account for the intra- and extravascular spaces. Volume space is quite complex. We often think of intravascular space, yet with our physical exam, we interrogate the extravascular space. Very often, an assessment of both can be of great value."
Redefining Cardiovascular Care: Leveraging Data and AI to Shape the Future of Medicine

Former FDA commissioner and current DCRI faculty member Robert Califf, MD, provided insight into the United States and global regulatory environment during a Saturday afternoon panel discussion focused on how artificial intelligence (AI) can be leveraged responsibly within cardiovascular care. He also shared what he referred to as “existential issues” that leaders in the field should be considering so that the advances serve to optimize benefits to patients, providers, and health systems.
To provide necessary oversight in how AI should be used, Califf recommended implementing a set of standards similar to those used to guide the farming industry.
“Just leaving things up to innovators is not a good idea, but too much oversight can be limiting,” he said. “We don’t tell farmers and grocery stores how to do things, we give them standards. If they adhere to those standards, it generally works.”
Looking ahead to what is next for AI, Califf highlighted two themes that leaders in the field need to consider:
- Clinicians are now spending a lot of time on documentation, which prevents them from spending time with patients and optimizing their care. AI can help with that, but when it does, will health system management require them to see more patients in the time that has been saved?
- If the AI decision systems advise something that is going to lose money for the health system or practice, how will health systems and clinicians handle these situations?
March 30 Sessions
Sacubitril+Valsartan Demonstrates Consistent Benefit Regardless of Structural Cardiac Abnormalities
Patients with heart failure with preserved ejection fraction (HFpEF) experienced a greater reduction in N-Terminal pro-B-type Natriuretic Peptide (NT-proBNP) with sacubitril plus valsartan versus valsartan alone regardless of the presence of structural cardiac abnormalities, according to an analysis presented by DCRI fellow Veraprapas "Mark" Kittipibul, MD, during a moderated poster session at ACC.
Kittipibul and colleagues conducted a post-hoc analysis of the PARAGLIDE-HF trial, examining how structural abnormalities, including left ventricular hypertrophy (LVH) and left atrial enlargement (LAE) affected treatment outcomes in patients with ejection fraction greater than 40% and worsening heart failure.
The researchers classified 454 patients (97% of the original study population) into three groups based on the severity of structural abnormalities: no LVH/LAE (26%), either LVH or LAE (39%), or both LVH and LAE (35%). The primary endpoint was time-averaged proportional change in NT-proBNP from baseline to weeks 4 and 8.
"We saw consistently greater reduction in antibodies across the restructuring group and a nonzero trend for greater intermediate production," Kittipibul said during his presentation.
Results showed that sacubitril plus valsartan provided greater NT-proBNP reduction than valsartan alone across all structural abnormality groups, with no significant interaction between treatment effect and degree of structural abnormalities (p interaction=0.70). However, they did note a trend toward larger NT-proBNP reduction with higher degrees of structural abnormalities.
Kittipibul noted that the study had limitations, including a relatively small sample size that could have limited statistical power for interaction testing. He suggested that future research further explore how structural cardiac abnormalities might modify treatment effectiveness in heart failure patients.
The PARAGLIDE-HF trial (NCT03988634) continues to provide important insights into treatment options for patients with HFpEF or mildly reduced ejection fraction. The trial represents potential advancement in treatment options for the condition, which historically has had fewer evidence-based treatment options than heart failure with reduced ejection fraction.
Advancing Medical Therapy for Older Adults With Ischemic Heart Disease
For older adults with ischemic heart disease, a condition where there is an inadequate blood supply to a part of the body, a conservative approach to therapy is not inferior to an invasive approach, according to DCRI’s Karen Alexander, MD, during a Sunday morning ACC presentation.
Alexander began by reviewing results from the ISCHEMIA study, which included more than 5,000 patients with moderate to severe ischemia, and compared conservative and invasive approaches, revealing no significant difference in outcomes. A later analysis showed that for quality of life and angina scores for older adults with ischemia, there was less improvement in older patients than in younger patients. The SENIOR-RITA trial further supported the efficacy of conservative medical therapy in patients over 75 with non-STEMI and cognitive impairment.
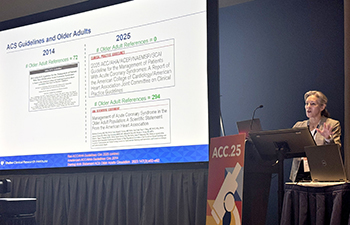
Alexander emphasized the importance of understanding the underlying risk of coronary artery disease (CAD) in older adults. She highlighted the MESA trial, which showed levels of coronary artery calcium (CAC) to be a strong predictor of cardiovascular risk among individuals aged 75 and older.
Alexander also introduced the PREVENTABLE trial, which studies the effects of atorvastatin in patients aged 75 and older. With 9,000 participants enrolled, the trial aims to determine whether statins can reduce dementia and disability in this age group.
Alexander discussed promising therapies on the horizon, including SGLT-2 inhibitors and incretin mimetics. These treatments have shown potential benefits in improving heart failure with preserved ejection fraction (HFpEF) and reducing major adverse cardiovascular events in older adults.
Alexander concluded by underscoring the need for further research into the shared drivers of aging and CAD.
“In older adults, a CON (conservative) strategy is pretty good,” Alexander said. “We can take some time and see if it will work. It's not inferior for even our higher-risk patients. Cardiovascular treatments may alter aging impairments as well, and we need to study that because of the shared drivers that we learn from geroscience, and I'm really hopeful that we'll learn more about these agents in the future.”
DCRI Faculty Highlight Cardiovascular Care Access Challenges, Opportunities
Barriers to cardiovascular care access extend well beyond the clinic visit, affecting millions of Americans who struggle to receive evidence-based therapies despite medical advances, according to DCRI's Manesh Patel, MD.
In a joint ACC symposium with leaders from major organizations focused on cardiovascular health, Patel outlined a growing cardiovascular disease crisis, with projections showing that 61 million Americans will have cardiovascular disease by 2050. Currently, 60% of U.S. counties lack a cardiologist, resulting in significant care disparities.

"Health systems vary widely in access to cardiovascular care," Patel said, highlighting that less than 10% of medical recommendations have full evidence-based support, and clinicians often prescribe therapies with limited evidence.
Even when evidence exists, effective implementation remains a challenge. Patel pointed to long-term follow-up studies from the SPRINT trial, which indicated that the benefits of intensive blood pressure control tended to diminish once the structured trial environment ended, underscoring the challenges of maintaining treatment adherence.
Several effective strategies have shown promise in improving access to care, including implementing pharmacist intervention programs, reducing medication copays, and creating structured care pathways. However, systemic barriers still exist and include unreliable patient information, insufficient primary care resources, and cognitive overload for clinicians.
Patel emphasized three key therapeutic areas where advancing implementation science could significantly enhance outcomes: high-intensity statins for atherosclerotic heart disease, glucagon-like peptide-1 (GLP-1) medications for weight management, and intensive blood pressure control strategies. Despite their proven benefits, these treatments remain underutilized.
Looking forward, Patel advocated for training the next generation of investigators in implementation research and encouraging health systems and payers to adopt new care models that scale evidence-based practices. He stressed that cardiovascular medicine's biggest challenge is not necessarily the discovery of new treatments but ensuring that patients can access these life-saving therapies.
March 31 Session
ACS Research Targets New Approaches for an Old Disease
As new therapeutic targets for acute coronary syndrome (ACS) emerge, implementing existing evidence-based therapies remains equally important, according to DCRI's Jennifer Rymer, MD.
During her presentation at ACC on new trends in ACS care, Rymer highlighted several promising research areas, particularly a renewed interest in the inflammatory pathway as a treatment target.

"As we explore new targets within our old hypotheses, it's essential to figure out how to implement current therapies and encourage patients to adhere to what we currently have available. We know that our rates of adherence and persistence to those currently approved medications need improvement," she said.
Rymer shared details of the ARTEMIS trial, which is investigating the monoclonal antibody ziltivekimab to reduce both acute and chronic inflammatory burdens in approximately 10,000 patients. This investigational medication targets the pro-inflammatory cytokine interleukin-6 (IL-6) and builds on promising efficacy data from Phase 1 and 2 trials.
In the area of antiplatelet therapy, Rymer discussed the SOS-AMI trial, which examines a novel subcutaneous P2Y12 inhibitor (selatogrel) that patients can self-administer during recurrent symptoms following hospital discharge. She pointed out the challenges associated with patient compliance when self-administering treatment during acute episodes.
Factor XI inhibitors were another area under investigation, although Rymer acknowledged the setbacks and early termination of the OCEANIC-AF due to stroke concerns. The LIBREXIA-ACS trial is now exploring an alternative approach with the factor XI inhibitor milvexian.
Lipid-lowering therapies continue to advance, with PCSK9 inhibitors showing promise in treating acute myocardial infarction. The EVOLVE-MI trial will assess the early use of evolocumab in combination with routine care versus standard care alone. Meanwhile, inclisiran showed significant reductions in low-density lipoprotein levels in the VICTORION-INITIATE trial.
Rymer concluded by emphasizing that while exploring new treatment targets remained important for advancing care, the medical community must also prioritize the implementation of currently approved therapies to improve patient outcomes.