One of the premier scientific meetings of the year with over 10,000 clinicians and researchers in attendance, the 2023 American Heart Association Scientific Sessions focused on the latest research and insights to improve cardiovascular health. This year’s event was held in Philadelphia, Nov. 10-13. The DCRI was represented in poster sessions, moderated digital poster sessions, debates, simulations, learning labs and main stage presentations.
See the full list of Duke and DCRI Sessions
Select Highlights from Day 1 — Saturday, Nov. 11
Title: Should All STEMIs Be Admitted to the CICU? No
Presenter: Jason Katz, MD/Christopher Granger, MD (Moderator)
Jason Katz, MD, participated in the Contemporary Debates in STEMI. This education session was planned by the Committee on Scientific Sessions Program and was moderated by DCRI’s Chris Granger, MD. The eight minute pro/con debates addressed controversial areas of addressing controversial areas of management in ACS. Particularly, this debate addresses an important issue in ICU care. Katz reviewed a few case studies that suggest implementing a risk-based triage strategy could be a better alternative to the current strategy where patients with STEMI are typically admitted to the CICU.
In summary, the CICU admission decision for STEMI patients will continue to be based on individual judgment and traditional protocols rather than robust and evidence-based risk prediction models.
Title: Temperature Control After Cardiac Arrest: A Shifting Landscape
Presenter: Konstantin Krychtiuk, MD, PhD

If you fall into ice cold water or get caught in an avalanche and go into cardiac arrest, you have a very good chance of survival with a good neurologic outcome, DCRI’s Konstantin Krychtiuk, MD, PhD, shared at the beginning of the session on cardiac arrest and CICU care. But there’s a catch: “Thing is, here we have hypothermia before cardiac arrest,” he said.
So, does hypothermia have the same effects on patients after cardiac arrest?
After reviewing data from trials spanning the last 25 years, Krychtiuk concluded that the evidence does not support hypothermic Targeted Temperature Management (TTM).
Though the guideline-changing but relatively small HACA trial in 2002 revealed that therapeutic hypothermia improved neurologic outcomes and reduced deaths in cardiac arrest patients, subsequent larger trials have done little to determine how it works or establish differences in the treatment’s application such as timing, temperature and duration.
“So, if we believe that therapeutic hypothermia works, but there’s no dose effect, no effect of duration, no effect of timing, the question is ‘does it actually work?’,” Krychtiuk asked.
Krychtiuk then compared more recent trials including a deeper dive into the TTM2 trial, which showed “virtually no difference” in outcomes between normothermia and hypothermia.
The differences observed with TTM in HACA, he speculated, could be from a more enhanced team-based systematic approach, by decreasing the premature withdrawal of life-saving methods, or by avoiding fever; and “probably not by hypothermia itself.”
“Overall, the totality of evidence, if you take everything together, does not support hypothermic TTM in 2023,” Krychtiuk said. “We need protocol-structured, supportive care, we need to prevent the withdrawal (of life support), and we need better evidence-base for structured neuroprognostication.”
Title: Bifurcation Disease: All You Need is One Stent
Presenter: Jennifer Rymer, MD, MBA

As part of a Saturday morning session examining controversies in high-risk PCI procedures focusing on calcium modification and bifurcation lesions, Jennifer Rymer, MD, MBA, participated in a debate on a one stent vs. two stent strategy for Bifurcation Disease, detailing scenarios in which a one stent approach would be appropriate.
Rymer emphasized that her position in favor of a provisional, one-stent strategy should be the default for many, but not all bifurcation lesions.
Pointing first to a meta-analysis of nine randomized controlled trials co-authored by her debate opponent Margaret McEntegart, MD, Rymer noted that the one-stent strategy showed reduced mortality compared to a two-stent strategy over a longer term follow-up.
Rymer reviewed further evidence from the Nordic bifurcation study, EBC Two, and EBC main trials, among others, showing that the provisional single-stent strategy was more favorable than a two stent strategy. Still, Rymer acknowledged that the one-stent strategy is not the definitive answer in every case.
“There’s significant evidence that a provisional stent strategy with often one stent can be a viable strategy for many bifurcation lesions,” Rymer said. “However, it’s key to assess and examine the anatomy and features of the bifurcation lesions, particularly within the left-main bifurcation. There isn’t always a one-size-fits-all-approach in any aspect of medicine and certainly in these lesions there’s not.”
In rebuttal, McEntegart largely agreed that a one-stent strategy is best when treating simple bifurcations, while highlighting the exceptions — when treating more complex bifurcations — in which a two-stent strategy is a better approach.
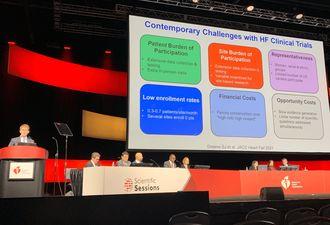
Title: Discussion/Wrap Up – Determining What is Best for Patients with Heart Failure: Novel Clinical Trial Designs
Presenter: Stephen Greene, MD
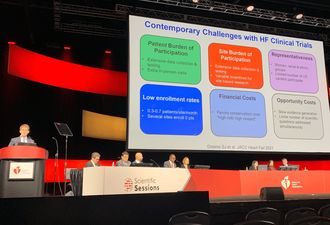
As a discussant for the late-breaking science session “Heart Failure – VADS, Kids, and Money,” Stephen Greene, MD, shared details of recent heart failure trials and reflected on how patient outcomes can be improved by treating heart failure with a greater sense of urgency, more efficient trial enrollment, and a focus on implementation.
He shared examples of innovative trial designs such as the CHIEF-HF study and TRANSFORM-HF trial that reduced burden on patients and sites, and then emphasized a focus on implementation as the missing link in heart failure outcomes.
“Even when we know what is quote-unquote best for patients — we know the answer, what makes them live longer, stay out of the hospital, feel better, spend more time at home with their families — history has told us that we do not routinely act on this information,” Greene said. “And, as a result, the grim reality is that every day in this country, many patients with heart failure are dying and being hospitalized without ever having the opportunity to receive medicines definitively proven to prevent these events, despite the patient being eligible for them.”
Greene cited “persistent and pervasive” gaps in use of guideline directed medical therapy, including less than one in 10 eligible patients being discharged on quadruple medical therapy, and less than one in three eligible patients going home on triple therapy.
“While of course quadruple therapy should be our goal for HFrEF patients, just think how much better off it would be for the heart failure community if we did complete, consistent and timely initiation of even just three generic heart failure medications,” Greene said.
“Traditional scientific investment in heart failure is largely focused on discovery science, and thankfully we’ve gotten enormous therapeutic advancements, but with these advancements comes the responsibility to get these therapies to our patients. … Regardless of any specific implementation strategy, there’s an overarching need to change the culture of care from therapeutic hesitancy to one of therapeutic urgency.”
Title: New Molecular Pathways in HFpEF: What Do They Tell Us for Developing New Therapeutic Targets?
Presenter: Marat Fudim, MD, MHS

Marat Fudim, MD, MHS shared predictions for the future of treatment for patients with heart failure with preserved ejection fraction (HFpEF) during an afternoon session packed with attendees eager to better understand what’s next. A more tailored approach with endo- and phenotyping, he said, is what will advance treatment for these patients, and machine learning may be able to help.
First outlining the need for more specialized research in HFpEF, Fudim noted that the subgroup makes up more than half the heart failure population and continues to grow. Yet the most helpful research for this subgroup has largely come by happenstance.
“In the past we have applied therapeutic successes from the HFrEF space, which is much easier to diagnose and conceptualize, and applied that to the heart failure preserved ejection fraction space,” Fudim said. “We’ve really seen no positive trials over the two decades that we’ve been testing it, until we started getting lucky with therapies which are actually primarily not cardio-centric — cardiometabolic drugs such as SGLT2s, GLP1RAs.”
But that approach will not be sustainable moving forward, he said.
“The future of HFpEF, I believe, will be looking as follows — we will have to do phenotyping,” Fudim said. “You can call it endotyping or phenotyping, and it will have to involve some form of superficial or deep phenotyping looking at clinical variables as well as biopsies or blood work that might tell us a little bit more about the patient, and then apply specific mechanisms of treatment to the diagnostically identified mechanism of pathology.”
Fudim provided the example of a case where spironolactone was found to be more therapeutically beneficial when matched it to the proper phenotypical group.
“Certain groups will simply benefit more from certain interventions, even possible interventions found not to be significantly beneficial,” he said.
Machine learning is already applied with screening echocardiograms, Fudim noted, and could also be useful in identifying specific disease processes and matching with specific drugs, as well as identifying patients for future clinical trials where specific endotypes or phenotypes could be matched to a specific drug.
Lesley Curtis, PhD, Receives Lifetime Achievement Award
Lesley Curtis, PhD, former Executive Director in the Duke Clinical Research Institute (DCRI), chief of the Department of Population Health Sciences and professor in the Duke School of Medicine Departments of Population Health Sciences and Medicine was presented with the QCOR Outstanding Lifetime Achievement Award by the American Heart Association’s Council on Quality of Care and Outcomes Research (QCOR). This award is presented to a Council member for their significant long-term contributions to outcomes research and the improvement of cardiovascular care.
Select highlights from Day 2 — Sunday, Nov. 12
Presentation Title: Pregnant Patients Should Undergo Catheter Ablation for Supraventricular Tacychardia to Avoid Drug Therapy: Con
Presenter: Sana Al-Khatib, MD, MHS

During an early morning Sunday session highlighting the pros and cons of controversial therapies for arrhythmia management in patients with complex clinical considerations, DCRI faculty member Sana Al-Khatib, MD, MHS shared evidence against catheter ablation for supraventricular tachycardia (SVT) in pregnant patients.
Following Kamala Tamirisa, MD, who took the “pro” position in favor of catheter ablation for SVT to avoid drug therapy, Al-Khatib argued that ablation should be avoided in these patients. Despite the presentation title, Al-Khatib cited guidelines and an expert consensus statement recommending that medications can and should be used to safely manage these patients. Al-Khatib went on to recommended that ablation could be considered either before or after pregnancy.
“Of course, I completely agree with my friend Dr. Tamirisa that we have to optimize the safety, we have to make sure that we know about the properties of these medications that we use, when we can use them, when we cannot use them, dose them appropriately, see if we can get away with lower doses,” Al-Khatib said. “In fact, many of us have been able to manage pregnant women with lower doses of these medications.”
Presentation Title: CHANGE of Beat in AFib: How Can Cardiologists and Electrophysiologists Navigate an Evolving Treatment Paradigm?
Presenter: Jonathan Piccini, MD, MHSc
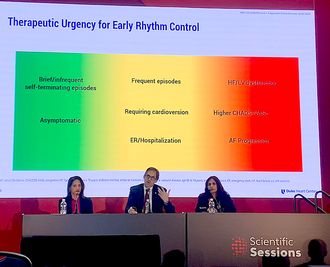
A lot has changed since the 2002 AFFIRM study showed a rhythm-control strategy offered no survival advantage over a rate-control strategy, according to Jonathan Piccini, MD, MHSc. On the contrary, data from more recent observational and randomized trials demonstrate that early initiation of rhythm control in patients with atrial fibrillation (AFib) can improve outcomes, Piccini said.
Presenting as part of a learning studio session on treating patients with AFib, Piccini reviewed recent evidence on early rhythm control such as the EAST-AFNET 4 trial, and discussed the applications of early rhythm control among different types of patients.
Which patients benefit most from early rhythm control?
“Some of the greatest benefit may be in patients who have more comorbidities,” Piccini said.
“I’d argue that we have good data that early rhythm control improves outcomes in persons with Afib and there appears to be a pretty durable 20% relative risk reduction in cardiovascular events. Persons with heart failure, left ventricular dysfunction, high degrees of comorbity, and who have AFib progression or who are at risk for developing AFib progression are particularly important candidates for early rhythm control.”
Presentation Title: Let’s get to the heart of it: Explore how evidence generation and select methodological approaches can help inform clinical practice in patients with nonvalvular atrial fibrillation (NVAF)
Presenter: Renato Lopes, MD, PhD
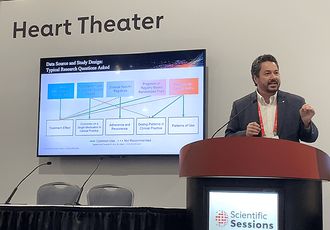
Renato Lopes, MD, PhD, detailed how randomized controlled trials (RCTs) and real world evidence (RWE) can help inform clinical practice, and shared examples of successful RCTs for atrial fibrillation.
“We always ask this question: What is the best type of study?,” Lopes said. “Is it randomized trials, or is it the real world type of study? …The right answer should be another question: ‘What is the question that I will answer?’ Because depending on the answer that I want to have from a clinical perspective, I might have different types of studies that might be the best.”
Randomized controlled trials are the gold standard for determining treatment effect, he said.
“I really need randomization to be able to define cause and effect relationships,” Lopes said.
However, for determining real-world application and understanding patterns of care — such as what dose people are using of a particular drug — real world evidence studies are a better approach. So, a combination of the two types of studies is helpful to support clinical decisions, he continued.
Lopes summarized two pivotal trials on atrial fibrillation with Apixaban — ARISTOTLE and AVERROES. Both RCTs, ARISTOTLE compared Apixaban to Warfarin, and AVERROES compared Apixaban against Aspirin. ARISTOTLE was able to show that Apixaban was not only non-inferior to Warfarin, but superior to it in terms of reducing stroke, risk of bleeding, and all-cause mortality.
“We couldn’t believe when we saw that we were able to meet every single endpoint of the trial. That’s what we call a homerun,” Lopes said. “To hit every single endpoint, preserving your alpha, was a really unique moment.”
Select highlights from Day 3 — Monday, Nov. 13
Presentation Title: Pro: Every Patient Should Have Rapid Titration of Quadruple Therapy
Presenter: Stephen Greene, MD
During a session on heart failure guidelines and implementation of therapies, Stephen Greene, MD, advocated for rapid titration of quadruple therapy for every eligible heart failure patient. Greene outlined the extreme risk associated with heart failure and emphasized the need for a more urgent therapeutic response. The status quo approach of introducing medications slowly using a one-move-at-a-time, serial, and selective approach, he said, has substantial risks associated as it can take 28 to 58 weeks before guideline directed medical therapy (GDMT) is fully implemented at the targeted doses.
Simultaneous or rapid-sequence initiation of GDMT, on the other hand, treats heart failure with the urgency that it deserves, he said, and the clinical benefits become noticeable within days to weeks.
“If you delay therapy, even a couple of weeks in an eligible patient, you’re exposing them to excess clinical risk,” Greene said. “And when you remember that the benefits of all four of these drugs are completely additive to each other, and when you further remember that we’re talking about an extreme risk condition that needs all the help it can get, we need to fully take advantage of these medicines ASAP.”
In rebuttal, University of Kentucky Healthcare’s Dr. Craig Beavers presenting on behalf of Alanna Morris, MD, argued that while the rapid titration approach is ideal, it wasn’t rooted in real-world thinking. Beavers outlined barriers to quadruple guideline-directed medical therapy for heart failure, including lack of provider knowledge, side effects, administrative burden, Medicare prescription drug coverage, high out of pocket costs and clinical inertia. He also outlined barriers to rapid titration therapy, including polypharmacy, side effects, financial toxicity, and patients failing to understand the rationale for changes.
Beavers concluded that while he agrees that an approach of rapid titration of quadruple therapy is needed for eligible heart failure patients, the current system is not set up to achieve it.
Presentation Title: Does Every Patient with Atrial Fibrillation Need Catheter Ablation?
Presenter: Jonathan Piccini, MD, MHSc
Presenting as part of an afternoon session on arrythmia treatment, DCRI’s Jonathan Piccini, MD, MHSc acknowledged that catheter ablation will not be needed by every patient. Most patients, though, will benefit from catheter ablation — “absolutely yes, beyond a shadow of a doubt,” he said.
Piccini went on to outline reasons to ablate — it can suppress atrial fibrillation, improve quality of life and reduce symptoms in patients.
“It’s not a cure, but it’s a highly effective form of suppressing active episodes of AFib,” Piccini said. “This forms the foundational pathophysiology and rationale on which catheter ablation is built.”
The EAST trial showed a 20 percent risk reduction in cardiovascular mortality, stroke, and hospitalization for both heart failure and coronary syndrome over five years, Piccini shared. In CABANA, the procedure showed similar risk reduction in deaths and cardiovascular hospitalization.
Like any procedure or drug prescribed in patients or intervention, applying it to the appropriate patients is critically linked to effectiveness and safety, he noted.
“Does every (AFib patient) need an ablation? No. But most people will probably benefit from ablation because at some point they will have symptoms. Or at some point they are going to benefit from rhythm control,” Piccini said. “EAST shows us that’s probably the beginning of their journey. … If we diagnosed it upfront and implemented early rhythm control, there is a very large role for catheter ablation in their health.”