
Faculty experts from the Duke Clinical Research Institute shared new research results, provided thought-provoking insights, and championed therapeutic guidelines and best practices as part of more than 40 sessions during the 2024 American Heart Association (AHA) Scientific Sessions.
The event, held in Chicago Nov. 16-18, honored the centennial anniversary of the AHA, celebrating a century of cardiovascular and stroke science.
In addition to the selection of highlights from DCRI faculty sessions noted below, the AHA Council on Quality of Care and Outcomes Research (QCOR) Council bestowed the Outstanding Lifetime Achievement Award on Adrian Hernandez, MD, MHS, the executive director of the Duke Clinical Research Institute (DCRI) and vice dean at the Duke University School of Medicine, during a reception on Nov. 16.
Click on the headlines below to navigate to a story:
Saturday, Nov. 16
- Health System Variability in Lipid Management for Patients with Atherosclerotic Cardiovascular Disease: An Analysis from Cv-MOBIUS
- Heating Up the Discussion: Key Debates in Acute Coronary Syndromes
- Exploring Bayesian Re-analysis: Insights from the Stress Trial
- Randomized Comparison of Left Atrial Appendage Closure with Oral Anticoagulation after Catheter Ablation for Atrial Fibrillation
- Improving Lipid Management Through Improved Utilization and Implementation Methods
- What’s New in Medical Therapies for PAD?
Sunday, Nov. 17
- Case Study: A Multifaceted Approach to Managing LDL-C, Triglycerides
- Advocating for Evidence-Based Approaches to Polypharmacy
- Exploring the Future of Heart Transplantation
- Glucagon-like Peptide-1 Receptor Agonist Use and Cardiac Outcomes in Patients with ESKD
- Contemporary Diagnosis, Management, and Outcomes of Patients with Low-Gradient Severe Aortic Stenosis
- Living on Borrowed Time: A Call to Action for Severe Aortic Stenosis Patients
- Targeting Underutilization of Key CV Medications with Effective Interventions
Monday, Nov. 18
- Advocating for Statins for Primary Prevention in Adults 75+
- Best Practices in Difficult Situations of Acute Coronary Syndrome
- Analyzing the PROMPT-AF Trial Late-Breaker at AHA
DCRI Highlights from AHA 2024
SATURDAY, NOV. 16

Health System Variability in Lipid Management for Patients with Atherosclerotic Cardiovascular Disease: An Analysis from Cv-MOBIUS
Health systems across the United States approach lipid management for patients with atherosclerotic cardiovascular disease (ASCVD) much differently, according to research shared by DCRI’s Nishant Shah, MD, as part of a moderated digital poster session on Nov. 16.
Researchers in the study reviewed the Cv-MOBIUS prospective registry of patients from 14 different health systems in diverse settings across the country over a two-year period beginning in January 2021. They identified more than 1 million patients from the registry who had ASCVD and reviewed their active prescriptions, biomarkers, and lipid parameters to assess variability in lipid management across the health systems.
The review revealed considerable variability in the use of combination therapy, monoclonal antibody proprotein convertase subtilisin/kexin type 9 (PCSK-9) inhibitors, ezetimibe, and more, Shah said.
“As an example, for high-intensity statin use across health systems, the proportion on a high-intensity statin varied from 18.9% to about 37.5%,” he said.
All of the health systems included identified as academic institutions, and many of them had dedicated lipid clinics and used algorithms to help with lipid management. Still, more than half of the patients were not on any statin or lipid-lowering therapy.
“Health systems varied widely in achieving LDL goals that are based on current guidelines,” Shah concluded. “The use of ezetimibe, PCSK-9 inhibitors, and monoclonal antibodies, at least, were very low across the health systems. There were low rates of achievement of an LDL of less than 70 mg/DL.
“What this data shows us, when you look across different health systems, is that there is significant variability in lipid-lowering across the country. Perhaps, we need to start thinking outside the box at innovative ways to place systems and care to help better our lipid-lowering therapy management.”
Heating Up the Discussion: Key Debates in Acute Coronary Syndromes
De-escalation — instead of abbreviation — of dual antiplatelet therapy (DAPT) can be a viable strategy, according to DCRI faculty member Jennifer Rymer, MD, MBA, during a debate about adjusting patient medication after a heart attack.
The science is not settled on whether these patients should be de-escalated from their high-intensity blood thinners to lower-intensity blood thinners in the months following a heart attack or whether simply shortening these therapies is a better approach.
Changing a patient’s medication can be challenging, Rymer said, and it can be difficult to know which of these patients are at the highest risk for another heart attack, death, or rehospitalization. De-escalating the medications too early can cause recurrent episodes or symptoms. Still, there is some evidence suggesting that de-escalation in the 3-to-12-month window after their heart attack could reduce their bleeding, she said.
“We have some good data to suggest that that would reduce bleeding from some of the trials that have been done, but we don’t fully have an answer of which patients we should de-escalate on or which patients we should just shorten therapy to less than 12 months,” she said. “Right now, physicians just do whatever is in their practice pattern without a lot of good data on what would actually reduce the bleeding risk in that patient.”
Rymer pointed to trials on platelet function testing and genotype testing which can help identify whether a patient is at a higher risk for coming off the medications.
“These trials have given us some data for reduction in bleeding if you are to use platelet function testing or genotyping to de-escalate,” Rymer said while noting that access to genotype testing can be a challenge. “A lot of places don’t have genotype testing capabilities, so it’s still a limited availability for that type of testing and can be quite expensive.”
The counterargument to de-escalation is to shorten the therapy overall, which could put patients at greater risk for another event.
Additional research, including studies using real-world data that phenotypes patients according to both risk and socioeconomic factors, would be helpful to create a more complete understanding and could lead to clearer guidelines and a more systematic approach to care across the United States.
Currently, approaches vary by practice and by region.
“Guidelines should move us away from that and to a more standardized process,” Rymer said. “I’m hoping that with real-world evidence, on top of trial data, we can get to a more algorithmic approach.”
Exploring Bayesian Re-analysis: Insights from the Stress Trial
The landscape of clinical trials is constantly evolving, with researchers continuously seeking more accurate and insightful methods to interpret data. In a recent presentation, Kevin Hill, MD, MS, shed light on the Bayesian re-analysis of the Steroids to Reduce Systemic Inflammation after Infant Heart Surgery (STRESS) trial, offering a fresh perspective on the trial's findings and underscoring the importance of alternative statistical approaches.
Hill emphasized that the lack of statistical significance should not be misconstrued as evidence of no effect. He referenced an influential editorial from Nature, which argued against the misuse and over-reliance on statistical significance in scientific research. The editorial advocated for a broader interpretation of data, beyond the binary notion of significance.
To provide a more nuanced understanding of the trial's outcomes, Hill introduced Bayesian analysis, an alternative statistical approach that evaluates the probability that one intervention is superior to another. Unlike traditional frequentist methods, Bayesian analysis incorporates prior knowledge and evidence, offering a probabilistic interpretation of results.
The Bayesian re-analysis of the Stress Trial revealed compelling insights. The analysis indicated a 91% probability that methylprednisolone provided some benefit compared to the placebo, with an estimated 13% average improvement in outcomes. These findings highlight the potential efficacy of methylprednisolone, despite the initial non-significant results.
Hill concluded his presentation by advocating for the broader adoption of Bayesian analysis in clinical research. He argued that this approach provides a more intuitive and comprehensive understanding of the probability of benefit, even though it involves complex computational methods. By embracing Bayesian analysis, researchers can gain deeper insights into their data, ultimately leading to more informed clinical decisions and better patient outcomes. The Bayesian re-analysis of the Stress Trial serves as a powerful example of how alternative statistical methods can enhance the interpretation of clinical trial data. As the field of clinical research continues to advance, incorporating diverse analytical approaches will be crucial in uncovering the true potential of medical interventions.
Randomized Comparison of Left Atrial Appendage Closure with Oral Anticoagulation after Catheter Ablation for Atrial Fibrillation
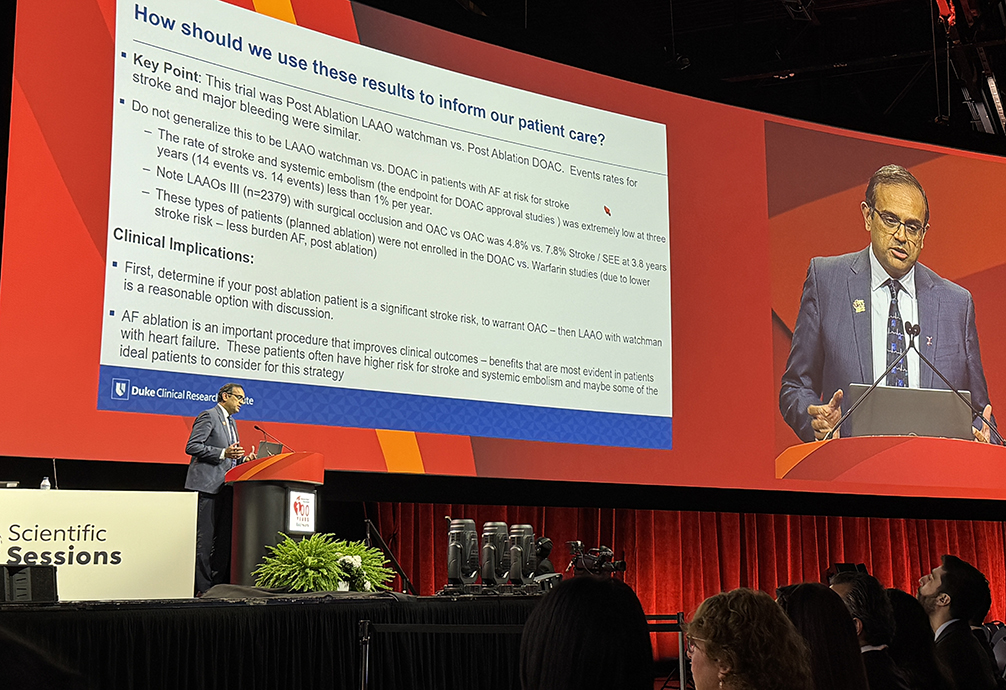
As a discussant for the OPTION study, DCRI’s Manesh Patel, MD, reviewed non-inferiority trial designs in atrial fibrillation (AF) and important considerations including assumptions, endpoints, and margins, before moving on to what was learned from OPTION and how clinicians could incorporate the results into their practice.
“We want to remember, as we think about non-inferiority trials, consistency of the endpoints, the estimated number of events we might have, and how we might put that into context in our practice,” he said.
Patel pointed to trials comparing direct oral anticoagulants (DOACs) to warfarin as an example. He reminded the audience about what was known on the topic before the trial, which showed that strategy was non-inferior for the primary endpoint. He also emphasized that the trial was on post-ablation patients.
“Don’t generalize this in all patients with AF,” he said. “Our discussion should be around post-ablation patients.”
Clinical implications, Patel shared, included determining if your post-ablation patient is a significant stroke risk to warrant anything, and if they do warrant something, then left atrial appendage occlusion with a Watchman implant is a reasonable option to discuss. He also noted that AF ablation is an important procedure that improves clinical outcomes, with benefits most evident in patients with heart failure. These patients often are at higher risk for stroke and embolism and may be some of the most ideal patients for this strategy.
Improving Lipid Management Through Improved Utilization and Implementation Methods
Emphasizing the urgent need for better implementation of low-density lipoprotein (LDL) management strategies, DCRI’s Neha Pagidipati, MD, MPH, referenced recent study results which revealed that only 40% of high-risk patients have an LDL of less than 70 mg/dL.
These findings from the CardioHealth Alliance REVEAL study also uncovered significant disparities, with female, Black, Hispanic, and peripheral artery disease (PAD) patients being less likely to have controlled LDL levels.
Despite the availability of effective lipid-lowering therapies, half of the U.S. patients with heart disease are not on any statin, and only 25% are on high-intensity statins. The study, which focused on LDL goal attainment among 200,000 patients with atherosclerotic cardiovascular disease (ASCVD) across five CardioHealth Alliance health systems, also found that only 20% of patients with uncontrolled LDL started therapy within six months.
"While it's important to talk about how we can improve the medications that we have, it's important to note that we're not even using what we have now," said Pagidipati. "And unfortunately, that's the case nationally."
To address these gaps, Pagidipati suggested several implementation strategies. At the clinician level, multidisciplinary team-based care, pharmacist and nurse-led interventions, and clinician education programs have shown promise. At the patient level, behavioral support, medication simplification, and reminders can help improve adherence. System-level strategies, such as electronic health record alerts and patient incentives, have modest impacts but are scalable.
Pagidipati also highlighted the CardioHealth Alliance's current Test to Treat program's objective of utilizing implementation strategies to improve LDL cholesterol testing and management for patients hospitalized for ASCVD.
What’s New in Medical Therapies for PAD?
DCRI’s Schuyler Jones, MD, discussed updated guidelines for peripheral artery disease (PAD) from the American College of Cardiology (ACC) and AHA Joint Committee on Clinical Practice Guidelines and provided insights on how the committee formulated its recommendations.

Jones — a liaison to the joint committee — opened by outlining the key components of medical therapy for PAD, including exercise, diabetes management, lipid-lowering therapy, hypertensive therapy, smoking cessation, and weight management. He also discussed the need to pay attention to risk amplifiers.
“We really do have to combat those things that sometimes we can control — chronic kidney disease, diabetes, hypertension, hyperlipidemia,” he said, adding that there are other risk amplifiers, such as advancing age, that are not controllable.
Included with the new guidelines was a list of the Top 10 Take-Home Messages, and Jones focused on the fifth item on this list: effective medical therapies, including antiplatelet, antithrombotic interventions and common risk amplifiers, and disease modifiers like lipid-lowering diabetes medications and hypertensives.
Guidelines for lipid-lowering therapy were among the recommendations he detailed, noting that one of the challenges for the committee is ensuring that guidelines are similar enough or in accordance with the cholesterol and diabetes guidelines. Within this context, he noted the Class 1 recommendation of high-intensity statins to lower patients’ low-density lipoprotein (LDL) by 50%.
“For those patients with LDL levels not less than 70, you can consider the use of other agents like ezetimibe and proprotein convertase subtilisin/kexin type 9 (PCSK-9s) to get below 70,” he said, noting that is a Class 2A recommendation from the committee.
Jones reviewed guidelines for hypertension management, including the Class 1 recommendation of using angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs).
Diabetes, he noted, is the area evolving the most quickly, and the committee had a deep discussion around the use of sodium-glucose cotransporter-2 (SGLT-2) inhibitors before coming to their Class 1A recommendation that these are effective to reduce the risk of major adverse events in these patients.
All of the ACC/AHA guidelines come with evidence gaps, Jones shared, adding that the evidence gap surrounding PAD is particularly large.
“We have to have better studies, and we have to generate data for patients as they’re treated — whether that’s for secondary prevention, or at the time of intervention, or to prevent intervention,” he said. “It’s critically important.”
“Medical therapies are paramount in how we care for our patients. We have to know how to prescribe it: these SGLT-2, glucagon-like peptide-1 (GLP-1) agents, as well as lipid-lowering therapies — these have to be in our arsenal. We have to keep pace with the times.”
SUNDAY, NOV. 17
Case Study: A Multifaceted Approach to Managing LDL-C, Triglycerides
While discussing a case study involving a middle-aged patient with obesity, diabetes, and elevated triglycerides, DCRI's Nishant Shah, MD, recommended a combination of lifestyle modifications, secondary cause evaluation, and lipid-lowering therapies to managing hypertriglyceridemia and hypercholesterolemia.
The patient, in their 40s, presented with slightly elevated blood pressure, diabetes managed with a sodium-glucose cotransporter-2 (SGLT2) inhibitor, an LDL level of 120 mg/dL, and triglycerides at 310 mg/dL. They were already taking ezetimibe and had several questions about cholesterol management and lifestyle changes.
"The approach that I recommend for managing triglycerides and LDL is multifaceted," Shah said. "It's not like you do one thing and then another thing. You have to do a lot of this all together."
Shah stated that he would include a comprehensive strategy that includes dietary restrictions and increased physical activity, evaluate the patient secondary causes, and use lipid-lowering therapies. Additionally, he noted the possible inclusion of therapies targeting triglycerides, such as omega-3 fatty acids, fibrates, and niacin.
One of the treatments Shah considered was icosapent ethyl, which has shown cardiovascular benefits in the REDUCE-IT trial and is FDA-approved for high-risk patients with triglycerides ≥150 mg/dL. He outlined the pros and cons of icosapent ethyl, noting its improved cardiovascular outcomes, plaque regression, and anti-inflammatory effects. However, he also noted that physicians should consider patients' concerns about the medication's cost and need for twice-daily dosing.
Other appropriate lifestyle modifications for physicians to consider include recommendations to minimize or abstain from alcohol, limit sweetened beverages, moderate fruit and vegetable intake, consume lean meats and fiber, and limit total fat to 10-30% of calories. Physical activity, such as 150 minutes of moderate or 75 minutes of vigorous exercise per week, can reduce triglycerides by up to 30%. Significant weight loss, defined as 5-10% of body weight, may also reduce triglycerides by up to 70%.
Shah recommended that physicians ensure patients with diabetes achieve optimal glycemic control by prescribing glucagon-like peptide-1 (GLP-1) agonists. Management should be based on fasting triglyceride levels, starting with statins and considering icosapent ethyl, with additional triglyceride-lowering therapies as needed. Lipid levels should be rechecked 6-12 weeks after intervention, with LDL treatment goals set at less than 70 or 55 mg/dL.
Advocating for Evidence-Based Approaches to Polypharmacy
During a debate on the value of deprescribing, DCRI's Adrian Hernandez, MD, MHS, made a compelling case for a more evidence-based approach to polypharmacy.

Polypharmacy, defined as taking over five prescribed medications a day, affects one-third of older patients, with no differences in gender or race. As the number of medications increases, so does the risk of adverse effects and lack of adherence.
Hernandez shared findings from a systematic review of 14 studies, which revealed that while deprescribing reduces the number of drugs used, it does not improve health-related quality of life, mortality, hospitalization, or emergency visits. Instead, he urged his colleagues to remain focused on therapies that truly benefit patients rather than just deprescribing for the sake of reducing medication counts.
"There are things we can do, and I wouldn't call it deprescribing," he said. "I would just say, 'Stop stupid drugs.'"
Hernandez offered session attendees possible alternatives for discontinuation or replacement while stressing the need for evidence-based practices and clear communication to avoid confusion about medications.
He highlighted the declining public trust in scientists and healthcare professionals, and the downward trend of life expectancy rates - down 2.8 years from the 2014 peak of 78.9 years.
"All of us are needed to stay strong with evidence," Hernandez said. "We need to be united right now. The evidence doesn't show anything about improved outcomes, and we already have enough problems."
Exploring the Future of Heart Transplantation
DCRI’s Adam DeVore, MD, MHS passionately advocated for the patient in a case study to be considered a prime candidate for transplantation during a Sunday morning session on heart transplants. With the patient experiencing advanced heart failure and a worsening condition, DeVore underscored the urgent need for a transplant to improve the patient's quality of life and prognosis.
Highlighting the remarkable growth of their transplant program, DeVore shared that his team now performs around 160 transplants annually. Impressively, this increase in transplants has not resulted in a reduction of left ventricular assist device (LVAD) procedures. This balanced approach demonstrates the program's strong preference for transplantation when feasible, ensuring that patients receive the best possible care tailored to their needs.
DeVore emphasized the critical importance of assessing a patient's resilience and their ability to tolerate immunosuppression post-transplant. In the case study, he noted that the patient had shown no signs of being unable to handle these post-transplant challenges, further supporting the case for transplantation.
Addressing the critical issue of organ availability, DeVore called for the transplant community to adopt more flexible donor acceptance criteria. He advocated for the inclusion of Donation after Circulatory Death (DCD) donors and other high-risk donors to increase the pool of suitable organs. This progressive approach aims to save more lives by expanding the criteria for donor acceptance.
In conclusion, DeVore strongly advocated for the patient in the case study to be considered for transplantation. He emphasized the importance of addressing reversible risks and adopting contemporary evidence-based practices to improve outcomes. His insights underscore the evolving landscape of transplantation, aiming to enhance patient care and optimize the use of available resources.
Glucagon-like Peptide-1 Receptor Agonist Use and Cardiac Outcomes in Patients with ESKD
A recent analysis by a DCRI fellow indicated that patients with end-stage kidney disease (ESKD) show significant improvement in nonfatal cardiac outcomes when treated with Glucagon-like Peptide-1 Receptor Agonists (GLP-1RAs). DCRI Fellow Benjamin Catanese, MD, shared his team’s findings during a moderated poster session at the American Heart Association (AHA) Scientific Sessions last weekend. GLP-1RAs may benefit high-risk ESKD patients who have few alternatives.
In clinical trials, GLP-1RAs have been shown to benefit patients with chronic kidney disease. Though these larger trials did not include patients with ESKD, smaller studies indicated that pharmacokinetics were favorable; meaning the kidneys were not involved in metabolizing the drug, and physicians began prescribing GLP-1RAs for patients on dialysis.
To evaluate the impact of GLP-1RAs in a patient population with both ESKD and Type-2 Diabetes, Catanese’s team obtained 10 years’ worth of data from the United States Renal Data System. They simulated a clinical trial, measuring a modified major adverse cardiovascular event (MACE) outcome based on rates of myocardial infarction, stroke, and all-cause mortality. The researchers compared patients who had been prescribed GLP-1RAs after starting dialysis to similar patients who had been prescribed dipeptidyl peptidase-4 inhibitors (DPP-4i), a drug that also lowers glucose but has not been shown to improve cardiovascular outcomes.
When it came to the modified MACE outcome, patients who were prescribed GLP-1RAs did not show significant improvement over those who were prescribed DPP-4is. This result was based on the MACE composite; when the research team turned to the individual components of outcome, they found that initiation of GLP1-RA was associated with significantly less nonfatal cardiovascular events.
“It provides good background data — that there is a benefit in this population that’s really sick,” Catanese said.
Many medications are ineffective when it comes to treating patients with ESKD, Catanese noted. These results indicate that GLP-1RAs could potentially benefit a high-risk group for which physicians don’t have a lot of other options.
Contemporary Diagnosis, Management, and Outcomes of Patients with Low-Gradient Severe Aortic Stenosis
An ePoster presented by Sreekanth Vemulapalli, MD, highlighted the differences in how aortic stenosis (AS) is assessed and managed across various US institutions.
The American College of Cardiology/American Heart Association guidelines recommend specific parameters for evaluating AS and suggest treating severe cases. However, real-world assessments of these guidelines are limited.
The study reviewed echocardiograms from 30 U.S. institutions between January 2018 and March 2024, revealing significant gaps in key evaluation metrics: Vmax (25% missing), mean aortic gradient (MG) (30%), aortic valve area (AVA) (35%), stroke volume index (83%), left ventricular ejection fraction (LVEF) (5%), and AS severity (36%).
Among 1,189,382 patients with severity assessments, 45,967 had severe AS, but only 52% were correctly diagnosed, and 20% were misclassified as having less severe AS. Of 26,903 patients with severe AS, more had low-gradient (LG) AS (52%) compared to high-gradient (HG) AS (48%). Fewer LG AS patients were evaluated by a Heart Team within 60 days (LG: 37%, HG: 53%) and received aortic valve replacement (AVR) within 6 months (LG: 35%, HG: 61%). Those not evaluated were generally older and more often female and non-White compared to those evaluated.
These findings emphasize the need to follow AS assessment guidelines closely and ensure all patients have equal access to evaluations and treatment, regardless of demographics. Vemulapalli's data highlights the importance of standardized diagnostic and treatment procedures to improve outcomes for severe AS patients.
Living on Borrowed Time: A Call to Action for Severe Aortic Stenosis Patients
Assessing and appropriately treating aortic stenosis (AS) requires a thorough assessment of the patient’s symptoms and a strong understanding of the parameters that define severe AS, according to Sreekanth Vemulapalli, MD, in a presentation that followed his Sunday poster session.

During his Nov. 17 afternoon session, Vemulapalli described keys to understanding symptoms and defining severity among patients, emphasizing the need to get it right so that these patients receive the care they need.
“You might think that symptoms are the simple part, but they really aren’t,” he began, noting that symptoms appear differently between men and women with aortic stenosis, and that supposed asymptomatic patients sometimes show symptoms when stress tested.
He shared a study of patients with severe AS who, according to their clinicians, were asymptomatic, but when exercising on a treadmill, 28% of those patients began to show symptoms.
“Symptoms on a treadmill were the number one predictor of whether they would develop symptoms in their daily life later on,” Vemulapalli said.
Providers should probe for patients’ true physical activity level and exercise intolerance, consult with one of their family members on these if possible, and consider exercise testing. He also urged clinicians to send overly complex cases to their heart team.
To determine whether a patient has severe AS, Vemulapalli said, understanding the definition, being sure that patients are being assessed correctly, and reporting patient severity properly are key.
Determining whether a patient has severe AS, means:
- measuring the mean gradient
- measuring peak velocity
- calculating the aortic valve area by measuring the left ventricular outflow tract diameter
- reporting the dimensionless index
“Even that may not be enough,” he said, noting that some patients meet the definition based on some, but not all, of these parameters. He said additional testing is needed for these discordant patients, pointing to a large recent study in which these measures were frequently excluded from reporting.
Vemulapalli closed by noting a need for consensus among providers about diagnosing severe and moderate-to-severe AS. “When there’s discordance, but patients had at least one symptom of severe AS, 52% of the time we called that severe, 28% of the time we called that moderate, 20% of the time we called it less than moderate,” he said. “So, one out of every two patients we’re misdiagnosing. Sometimes, in one out of every five patients, we’re calling it ‘mild’ or less.”

Targeting Underutilization of Key CV Medications with Effective Interventions
DCRI's Neha Pagidipati, MD, MPH, highlighted the significant underutilization of key cardiovascular medications among patients with diabetes and atherosclerotic cardiovascular disease (ASCVD).
Despite the proven benefits of newer medications, only 20-25% of these patients are on high-intensity statins, half are on angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs), and less than 10% are on sodium-glucose cotransporter-2 (SGLT2) inhibitors or glucagon-like peptide-1 (GLP-1) receptor agonists.
Pagidipati showcased findings from the COORDINATE-Diabetes study and the DRIVE trial, demonstrating substantial improvements in prescription rates through targeted interventions. The COORDINATE-Diabetes study, a cluster-randomized trial conducted in 43 cardiology clinics, tested a multi-faceted intervention that included assessing local barriers, utilizing pharmacists, coordinating care, and providing data feedback to sites. At baseline, none of the patients were on all three medication classes. However, after 6-12 months, 38% of patients in the intervention arm were on all three classes of medications, compared to 15% in the usual care group.
The DRIVE trial, a remote, randomized, non-traditional intervention trial, aimed to improve the prescription of SGLT2 inhibitors or GLP-1 receptor agonists in patients with diabetes and either cardiovascular or kidney disease. The trial utilized non-licensed navigators and clinical pharmacists, some of whom were college students, to achieve high prescription and adherence rates. The navigators partnered with clinical pharmacists who could prescribe the medications. Prescription rates reached 64% across both arms, significantly higher than the 10-15% rates observed in the COORDINATE study.
A Veterans Health Administration study also showed better numbers but still demonstrated significant variation — 11% on SGLT2s and 8% on GLP-1s, with younger, white patients more likely to receive both.
Pagidipati emphasized the need for broader implementation of these interventions to improve medication use.
"We're not using these drugs enough, and we should be," she said. "We're learning ways, on system levels, to help improve the use of these medications. Now, we need to understand how to spread, disseminate, scale, and sustain those interventions. That's the next frontier."
MONDAY, NOV. 18
Advocating for Statins for Primary Prevention in Adults 75+
DCRI's Karen Alexander, MD, made a compelling case for statins for primary prevention in adults 75+ during a friendly debate with Weill Cornell's Parag Goyal, MD, MSc.

Heart disease and dementia are significant concerns in late life, and data suggests that statins may reduce cardiovascular events, particularly in those with coronary artery calcification. Alexander argued that statins are both inexpensive and readily available, making them scalable for wider use. Many adults begin taking statins in middle age, and continued use into older age appears logical.
In her presentation, Alexander emphasized the importance of late-life prevention, noting that older adults are a heterogeneous group with diverse health concerns. She highlighted that statins are effective for secondary prevention of cardiovascular disease regardless of age, but there is uncertainty about their use for primary prevention in the 75+ population.
"Regarding statins for late-life prevention, I say yes, absolutely," she argued. "However, we know we're probably continuing and/or initiating them unevenly in relation to their benefit. What we need to do with better evidence is to get to a future state where we truly know who's going to benefit from a statin and who will not for expected future health concerns."
Goyal, on the other hand, pointed out the high rates of polypharmacy among older adults, which can lead to treatment burden, under-prescribing, non-adherence, and increased risk of adverse drug events. He argued that there is no strong evidence that individuals aged 75+ without cardiovascular disease need to start a statin at this stage and suggested focusing on lifestyle interventions instead. Goyal also recommended considering sodium-glucose cotransporter-2 (SGLT2) inhibitors as an alternative for primary prevention in older adults, as they may provide greater benefits than statins.
Alexander and Goyal are co-investigators on the PREVENTABLE study, which aims to determine if statins can prevent dementia and disability in the 75+ population. The randomized approach includes adults without existing cardiovascular disease, dementia, or disability and assigns them to either a statin (atorvastatin 40mg) or a placebo. The primary outcome is survival free of new dementia or persistent disability, with a secondary outcome focusing on cardiovascular events.
Both investigators encouraged attendees to consider enrolling eligible patients in the PREVENTABLE study to help advance the science.
Best Practices in Difficult Situations of Acute Coronary Syndrome
In a Monday morning session about best practices in difficult cases of acute coronary syndrome (ACS), DCRI’s Jennifer Rymer, MD, MBA, provided additional insights and guided discussion around best practices for managing extensive intracoronary thrombus and multivessel disease. Her insights included timing for stent placement and whether to fix non-culprit lesions.
Responding to an audience question about how to maximize pharmacologic therapy for patients with untreated non-culprit lesions who are often lost to follow-up, Rymer reflected on her experience doing procedures in a rural, underserved community. She urged the audience to consider patient access and affordability when prescribing so that patients are set up for success.
“I’m very sensitive to these issues because I think a lot of times, we underappreciate how little funds our patients have, and how many medications we’re starting them on,” Rymer said, running down a list of post-ACS agents that include high-intensity statins, dual-antiplatelet therapy. “We’re really good about checking off all of those boxes as to what medications we should start, but we’re not great about thinking ‘how much is that costing?’”
She noted that patients will sometimes come back after a procedure, sharing that their medications are too costly so they’re not taking them.
Rymer recommended that clinicians talk with their patients and collaborate with their hospital colleagues to better understand costs and develop treatment plans with consideration for interventions that are accessible and affordable to help keep patients on track.
“Really making sure you’re not only thinking about the right medications, but can they afford them, can they get them, and are they going to take them,” she said.
Analyzing the PROMPT-AF Trial Late-Breaker at AHA
Following an overview of the PROMPT-AF late-breaking results at AHA, DCRI's Jonathan Piccini, MD, MHS, gave his own in-depth assessment of the significance of the pivotal study that confirms the efficacy of a more extensive ablation strategy as a significant treatment option for patients with persistent atrial fibrillation (AF).

It is the first study to investigate the effectiveness of an optimized linear ablation strategy beyond pulmonary vein isolation (PVI).
PROMPT-AF compared a linear ablation strategy including the mitral isthmus line, left atrial roof line, and cavotricuspid isthmus line, combined with a vein of Marshall alcohol infusion (EIVOAM), versus PVI alone. The results demonstrated that the linear ablation plus EIVOAM significantly improved freedom from any atrial arrhythmia compared to PVI alone, with a 17.7% versus 61.5% success rate at one year.
Piccini noted that while the PROMPT-AF trial confirms the efficacy results from the VENUS trial, it also raises critical questions about patient selection and the potential benefits for those treated with pulsed-field ablation, an emerging technology for AF.
"Thus, there's a critical unanswered question in our field: is PVI with linear ablation and vein control alcohol infusion superior to a strategy of PVI only and patients with persistent atrial fibrillation?" he asked.
The trial randomized 495 patients with early persistent AF to either PVI plus linear ablation (roof, mitral isthmus, cavotricuspid isthmus) and vein of Marshall alcohol infusion, or PVI alone. The combined intervention was associated with a 9% absolute improvement in one-year rhythm maintenance.
Strengths of the PROMPT-AF trial, Piccini said, include its large, adequately powered randomized controlled trial design and the achievement of vein of Marshall alcohol infusion in 85% of eligible patients. However, limitations include a relatively "robust" patient population with a medium-sized left atrial diameter, which may limit the generalizability of the results to the broader persistent AF population seen in clinical practice. Additionally, the complication rate was double in the PVI plus linear ablation and alcohol infusion arm compared to the PVI-only arm, highlighting an important tradeoff to consider.