
The Duke Clinical Research Institute (DCRI) had a broad and visible presence throughout the 2025 American Heart Association Scientific Sessions, Nov. 7-10 in New Orleans. Faculty and staff participated in more than 40 sessions across a wide spectrum of scientific and educational sessions. Their contributions spanned general and featured presentations, moderated discussions, digital poster forums, late-breaking and featured science, and hands-on simulations. DCRI experts served as presenters, panelists, moderators, social media hosts, and poster professors as they presented new results, synthesized best practices, and shared insights into clinical practice.
Collectively, their work covered an extensive range of topics, including nearly every major cardiovascular subspecialty, underscoring the DCRI’s broad impact across the field.
Browse highlights from the DCRI’s thought leadership at AHA below, or view the full list of DCRI’s sessions.
Friday, Nov. 7
- Running on Empty: How New Therapies Help the Failing Heart Refuel
- In a Time of Widespread Misinformation in Healthcare, DCRI's Califf Encourages Advocating for Values
Saturday, Nov. 8
- Navigating Complexity: How Interdisciplinary Teams and Care Coordinators Improve CKM Outcomes
- ATTR-CM Patients Face Greater Risk of HF Readmission and Higher Healthcare Costs
- Mortality Rates and Causes of Death in Patients with CHD Across the Lifespan
- Study Links Biomarkers to Mortality Risk for Infants with Single Ventricle Heart Disease
- Finding a Balance: Reducing Risk of Bleeding, Maintaining Efficacy While Shortening DAPT in Patients with ACS
- Catheter Ablation May Improve Cognitive Function in Patients with Atrial Fibrillation
- Clinically Stable ASCVD Patients Are Undertreated for LDL-C
- Patel Highlights Complexity of Noninferiority Trial Design and Clinical Implications of OPTIMA-AF Study
Sunday, Nov. 9
- Initial Data From First in Human Gene Therapy Trial Supports Safety, Advance To Phase 2 Trials
- HeartSafe Workplace Initiative Supports Broad CPR Training Efforts Through Businesses
- RNAi Therapy Zilebesiran Demonstrates Safety in KARDIA-3, Advances to ZENITH Outcomes Trial
- GLP-1RAs Have Potential to Improve Health Broadly at Population Level, but Currently Being Underprescribed
- Rymer Brings Peripheral Procedure Expertise to AHA Simulation Zone
Monday, Nov. 10
- Leadless Pacemakers: Transformative Cardiac Care for High-Risk Patients
- The Economic and Clinical Argument for Hospital at Home Care Model for Heart Failure
Friday, Nov. 7
Running on Empty: How New Therapies Help the Failing Heart Refuel
The heart has high energy demands, DCRI’s Svati Shah, MD, MHS, emphasized during an early morning presentation on AHA’s opening day, and the failing heart is like an engine out of fuel.
During the session “Heart Failur-omics,” Shah described the varying fuels used by the heart, how the balance among them becomes disrupted in heart failure, and the effects of key types of therapies in the cardiologist’s tool chest.

“While fatty acids and glucose are the primary sources of fuels during times of stress, even in the resting heart, the heart can also utilize alternative fuel sources like branched chain amino acids and ketones,” Shah said, adding that the understanding of ketones has evolved in recent years, and they may be more beneficial than previously thought.
“In humans, mechanistic data have shown that even mild to moderate ketosis can have pleiotropic beneficial effects on the heart,” she said, listing improvements in endothelial function, oxidative stress, mitochondrial function, and inflammation among the benefits.
Evidence shared included a small study of 24 patients with heart failure with reduced ejection fraction (HFrEF), suggesting that a ketone ester drink improved key markers of heart function, and studies led by Senthil Selvaraj, MD, MS, MA, suggesting that these work together with SGLT2 inhibitors to help the heart use its fuel more efficiently.
“We saw marked changes in a majority of the metabolites, including reductions in medium and long chain acylcarnitines, which reflect fatty acid metabolism, suggesting that with this ketone ester drink you have more availability of ketones, and you have less reliance on fatty acids,” Shah said.
Shah also shared data suggesting that GLP-1 receptor agonists (GLP-1RAs) have benefits on fatty acid oxidation and building understanding of the therapies’ multidimensional pathways of improving other heart health indicators.
“SGL-2 inhibitors have benefits that may not be mediated only through their effects on ketones,” Shah said. “Key fuels substrate metabolic pathways, including fatty acids and ketones, are dysregulated in heart failure, and metabolic modulation of heart failure is a promising avenue for therapeutics and personalized medicine.”
In a Time of Widespread Misinformation in Healthcare, DCRI’s Califf Encourages Advocating for Values

A session focused on the potential effects of the One Big Beautiful Bill Act through the lens of cardiovascular health included several presentations detailing sobering evidence pointing to drastic loss of coverage through Medicare and Affordable Care Act cuts, the destabilization of health care in rural areas, and increased deaths.
DCRI founding director and former FDA commissioner Robert Califf, MD, spoke as part of a panel following these presentations, emphasizing U.S. health outcomes lagging behind other high-income countries, with a widening gap due to disparities. Califf was sitting next to another former DCRI director, Robert Harrington, MD, and the conversation shifted to the prevalence of misinformation and the importance of finding ways to counter it. Both Harrington and Califf emphasized the need for individuals to advocate for their values and share data within their communities through personal interactions and social media.
“I think it really is an important point in our history and a time for people to declare what their values are, whether they're in a leadership position or in a position of just doing their work,” Califf said.
Saturday, Nov. 8
Navigating Complexity: How Interdisciplinary Teams and Care Coordinators Improve CKM Outcomes

Patients with cardiovascular-kidney-metabolic (CKM) syndrome don’t fail therapies—systems do.
That was the message from DCRI’s Neha Pagidipati, MD, MPH, who called for interdisciplinary care models to help patients navigate an increasingly complex landscape of evidence-based treatments.
Pagidipati emphasized the critical role of CKM coordinators and shared practical strategies for streamlining care during two presentations at AHA 2025.
“Somebody has to be in charge and help the patient walk through this really complex system,” she said.
Pagidipati emphasized the importance of interdisciplinary care models and the shift from volume-based to value-based care, noting that individual patient risk level should guide the approach.
For low-risk patients, she said that coordinated visits from multidisciplinary teams without multiple subspecialist visits can be the right approach. For high-risk patients, CKM coordinators remain essential to ensure guideline-based therapies are implemented across subspecialists.
She stressed the need to work within real-world constraints, leveraging existing personnel and systems rather than waiting for ideal conditions or specific funding.
“There is no one right way,” she said. “The whole point is that there are as many ways as health systems. But there needs to be coordination and someone who cares.”
Pagidipati highlighted several examples of interdisciplinary care teams conducting interdisciplinary care coordination, including Duke’s Cardiometabolic Prevention Clinic and programs like CINEMA and the CardioMetabolic Center Alliance, which underscore the pivotal role of a care coordinator or navigator.
“Patients need more than just good medicine. They need good systems to be able to deliver that,” Pagidipati said.
ATTR-CM Patients Face Greater Risk of HF Readmission and Higher Healthcare Costs
Among older adults hospitalized for heart failure (HF) in the United States, patients with transthyretin cardiac amyloidosis (ATTR-CM) experience similarly high rates of post-discharge mortality, but face a greater risk of HF readmission and accrue higher post-discharge healthcare costs.

DCRI fellow Satoshi Shoji, MD, presented these results, highlighting the disproportionate clinical and economic burden of ATTR-CM compared with the general HF population.
Using data from more than 505,000 admissions across 600 U.S. hospitals (2021–2024) and Medicare datasets, researchers analyzed one-year outcomes, including mortality, readmissions, and healthcare costs.
ATTR cardiomyopathy was associated with a higher risk of heart failure readmission, but not with all-cause mortality or overall readmission. These patients incurred significantly higher healthcare costs, primarily driven by outpatient services.
“Medication costs were excluded, meaning the true economic burden may be even greater,” Shoji said. “The study highlights the need for enhanced strategies to implement therapy that improves outcomes while providing high-value care.”
Mortality Rates and Causes of Death in Patients with CHD Across the Lifespan
A recent study provided a greater understanding of mortality rates and causes of death in patients with congenital heart disease (CHD) across the lifespan.
The team, led by DCRI fellow Allison Levin, MD, MSc, analyzed data from more than 218,000 patients aged 0–45 years across seven states between 2010 and 2019. CHD was grouped into two types: severe (sevCHD) and non-severe (nsCHD).
Levin presented the results at AHA, revealing that mortality is highest in infancy for both sevCHD and nsCHD. Around 3% of all patients died during the study, and the risk was much higher for those with severe CHD (8%) compared to those with non-severe CHD (2%). For babies with severe CHD, the death rate was extremely high compared to those with milder forms.
This represents the most comprehensive U.S. population-based analysis of mortality rates (MR) and causes of death (COD) among patients with congenital heart disease (CHD) to date.
The data showed that as patients age, deaths were still more common in patients with severe CHD, but the official causes changed. In younger patients, most deaths were caused by CHD itself. In adults over 40, both CHD and acquired heart problems like heart attacks and strokes were major causes. Heart failure became a leading cause of death in older age groups.
“For the first time at a population-wide level, we really gained some hard estimates of mortality over the lifespan in these CHD populations,” Levin said. “We’re really advocating for closer monitoring of acquired heart disease that can happen in these patients.”
Watch Levin Discuss Her Insights
Study Links Biomarkers to Mortality Risk for Infants with SVHD

A recent study led by DCRI’s Elizabeth Thompson, MD, found that natriuretic peptide NT-proBNP and MR-proANP may serve as biomarkers to help identify high-risk infants with single ventricle heart disease (SVHD).
These infants face increased risk of morbidity and mortality during the time between the first and second of three palliative surgeries necessary in their first years of life.
The research team collected plasma samples from 50 infants across 10 sites. Using nonlinear, mixed-effects modeling, they characterized biomarker trajectories and their association with clinical outcomes.
The analysis identified a biexponential decline in biomarker levels, showing that concentrations dropped substantially during the first month after the first surgery, then slowed. Infants who died had higher coefficients for the slow elimination phase, suggesting persistent myocardial stress.
“Ultimately, we hope that this can translate into clinical practice by measuring levels of NT-proBNP, seeing how they trend over time, comparing them to our model, and being able to intervene when kids are at a high risk,” Thompson explained.
Finding a Balance: Reducing Risk of Bleeding, Maintaining Efficacy While Shortening DAPT in Patients with ACS
Shortening aspirin use among patients with acute coronary syndrome who are also taking a P2Y12 inhibitor can reduce bleeding risk, but how soon is too soon?

Renato Lopes, MD, PhD, highlighted the complexity of antithrombotic therapy for patients with acute coronary syndrome (ACS), sharing strategies for shortening the duration of dual antiplatelet therapy (DAPT) in favor of monotherapy to reduce the risk of bleeding in these patients.
“When you bleed, it’s a marker of worse prognosis,” Lopes said.
Studies reviewed included the TWILIGHT, STOPDAPT-2 ACS, and NEOMINDSET trials, which explore how short DAPT can safely be while maintaining thrombotic protection.
Lopes emphasized the importance of reducing bleeding risk while preserving the efficacy of the therapy to reduce the risk of stroke.
Despite evolving scientific understanding, real-world practice has not kept pace.
“People are stopping the P2Y12 inhibitor and continuing aspirin, but now we have enough data showing that it's probably better to continue the P2Y12 inhibitor and not the aspirin for the chronic patients,” Lopes said.
He concluded that more evidence is needed in this space, and implementation should better align with the existing data.
Catheter Ablation May Improve Cognitive Function in Patients with AF

The effects of atrial fibrillation (AF) extend beyond how well the heart itself is functioning. DCRI’s Jonathan Piccini, MD, MHS, highlighted AF’s strong associations with reduced brain volume and the condition’s capacity to impair cognitive function.
Piccini shared evidence showing that catheter ablation can help improve cognition and that ablation is superior to medical therapy for improving anxiety and depression in patients with AF. He also acknowledged dissenting data, presenting findings indicating that some patients may experience cognitive dysfunction after ablation; those effects, he noted, improved at one year. He emphasized the need for randomized trials for further clarity.
A current Duke study — NOGGIN AF — is evaluating how to best maintain and improve brain function in patients with AF. The study is comparing neuroanatomic changes and neurologic function in people undergoing rhythm control with ablation vs. medical therapy over 18 months. It will observe cortical thinning, brain blood flow, cognitive function, functional MRI, and AF burden.
“So much of our time is spent focusing on keeping people in sinus rhythm, and I think that is critical,” Piccini said, “but it is high time for us to be looking beyond that horizon and looking at preserving critical and organ health, and the brain certainly is no exception to that.”
Watch Piccini Summarize These Findings
Clinically Stable ASCVD Patients Are Undertreated for LDL-C
Many people with atherosclerotic cardiovascular disease (ASCVD) are not reaching recommended low-density lipoprotein cholesterol (LDL-C) goals, even after years of treatment, according to findings shared by DCRI fellow Satoshi Shoji, MD.
Using data from the cvMOBIUS-2 registry, which included 414,000 patients at 17 major U.S. hospitals, researchers found that average LDL-C decreased from 98 mg/dL to 83 mg/dL over about 28 months. While this represents progress, 70% of patients remained above 70 mg/dL, and 87% were above 55 mg/dL—the recommended level.
Patients with Medicaid insurance and those who had not had another heart-related event were more likely to have persistently high LDL-C.
“These findings highlight a critical need to both longitudinally monitor and practically intervene, as these data suggest that clinically stable patients are undertreated,” Shoji said.
Patel Highlights Complexity of Noninferiority Trial Design and Clinical Implications of OPTIMA-AF study
AHA President-elect and Duke Health Chief of Cardiology Manesh Patel, MD, offered a thoughtful and nuanced discussion of the OPTIMA-AF trial, emphasizing the complexity of noninferiority trial design and implications for managing atrial fibrillation (AF) patients undergoing percutaneous coronary intervention (PCI).
The OPTIMA-AF trial, conducted in 1,000 Japanese patients, demonstrated that a simplified regimen of clot-preventing medication after stent placement could be as safe and effective as the standard year-long approach.
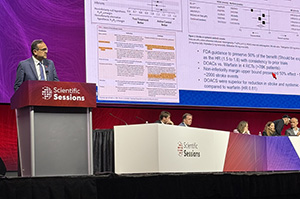
Standard post-stent therapy includes a direct oral anticoagulant (DOAC) — such as dabigatran, rivaroxaban, apixaban, and edoxaban to help prevent strokes; and a P2Y12 inhibitor, such as clopidogrel or prasugrel, a combination that can increase bleeding risk.
The analysis found that 5.4% of participants in the one-month group and 4.5% in the 12-month group experienced a heart attack, stroke, or death, suggesting similar efficacy with fewer bleeding complications.
Patel emphasized these trials rely on preserving a portion of the established benefit, often expressed as hazard ratios.
"Noninferiority trial designs are often complicated to understand, and determining if something becomes inconclusive is critical," he said.
In practice, he recommended continuing DOAC-based strategies and tailoring the therapy duration to a patient’s individual ischemic and bleeding risk.
He also highlighted FDA guidance recommending preservation of 50% of the drug warfarin’s benefit. Patel concluded that OPTIMA-AF offers valuable insights but requires careful application in clinical decision-making.
Sunday, Nov. 9
Initial Data from First-in-Human Gene Therapy Trial Supports Safety, Advances To Phase 2 Trials

Initial data from a first-in-human gene therapy trial for patients with heart failure with preserved ejection fraction (HFpEF) support progression to a phase 2 trial, according to DCRI’s Marat Fudim, MD, MHS, who presented during a late-breaking featured science session.
Fudim explained the rationale for targeting excitation-contraction coupling in myocytes, focusing on the role of the SERCA2a protein as a calcium cycling pump, and described how its underexpression in heart failure impairs contraction and relaxation, thereby justifying the gene therapy approach.
The MUSIC HFpEF study has now enrolled all patients in both cohorts, with low and high-dose therapy.
Fudim’s presentation on Saturday focused on the first five patients from Cohort A — the lower dose cohort — who are the only ones thus far to have completed the entire 12-month follow-up period.
Among these patients, no severe adverse events related to the drug, infusion, or procedures were observed, and significant improvements in wedge pressure at rest and with exercise were observed over 12 months, with no new medications introduced.
“At the 6-month mark, you have very little change from baseline in this treatment cohort, and then in the 12-month cohort, you had an improvement of around 30% at rest and with peak exercise, which equated to a -4.1 mmHg change at rest or 9.3 mmHg change with exercise,” Fudim said. “Now these are very large changes, believe it or not, in the space of exercise hemodynamics.”
If confirmed in future studies, Fudim shared that the pulmonary capillary wedge pressure improvement could suggest the potential for improved HFpEF outcomes.
Watch Fudim Share His AHA Highlights
HeartSafe Workplace Initiative Supports Broad CPR Training Efforts Through Businesses
Sudden cardiac arrest is a leading cause of death in the United States, but bystander CPR rates remain low. A team of researchers from the DCRI, in partnership with EMS agencies, hospitals, 911 dispatch, fire, rescue, law enforcement agencies, and communities throughout North Carolina, is working to improve response rates and save more lives.

DCRI’s Tyler Cope, DPT, shared a key piece of that RACE-CARS Trial team’s efforts — called the HeartSafe Workplace initiative — during a Sunday afternoon poster session.
The team is partnering with counties to support and incentivize their largest and most engaged businesses to accomplish two tasks:
- train all employees in hands-only CPR, and
- maintain a cardiac arrest emergency action plan.
The program provides the counties with toolkits supporting training, implementation, and recognition for the workplaces that meet those two criteria.
After roughly one year, 21 of the 30 targeted counties have adopted the program, and 79 workplaces have earned the initiative’s HeartSafe Workplace recognition. Participating counties reported about 150,000 employees trained in CPR so far.
“To truly move the needle in bystander CPR rates and survival rates, you need to train tens to hundreds of thousands of people trained in CPR to see a population-level impact,” Cope said. “I think that this framework is completely scalable outside of this trial.”
In February 2026, the team plans an attempt to break the world record for the most people trained in CPR in one day, aiming to engage many more workplaces.
RNAi Therapy Zilebesiran Demonstrates Safety in KARDIA-3, Advances to ZENITH Outcomes Trial
Despite the availability of blood pressure-lowering medications, many patients struggle to achieve and maintain adequate control of their blood pressure. The KARDIA-3 study is examining a novel therapy’s effects in hypertensive patients and those with high cardiovascular risk.
Single doses of the novel, long-acting RNA interference (RNAi) therapy zilebesiran demonstrated an acceptable safety profile Cohort B, according to data presented by DCRI’s Neha Pagidipati, MD, MPH, during a late-breaking featured science session.
Cohort B included individuals with cardiovascular disease or at high risk who have uncontrolled hypertension, are on multiple antihypertensive medications, and have chronic kidney disease.
Pagidipati reported that most adverse events were mild to moderate, with low rates of kidney dysfunction, hyperkalemia, and hypotension. No evidence of dose-dependent adverse effects emerged, and Phase 2 data support the use of the 300mg dose.
These Cohort B results follow Pagidipati’s Hot Line presentation of KARDIA-3 results at the European Society of Cardiology Congress, where she reported clinically meaningful reductions in office systolic blood pressure at the three-month primary endpoint, with sustained control through six months.
The now-enrolling ZENITH trial will evaluate the impact of zilebesiran on CV outcomes in patients with hypertension and established CV disease or high CV risk.
GLP-1RAs Have Potential to Improve Health Broadly at Population Level, but Currently Underprescribed

GLP-1 receptor agonists (GLP-1 RAs) have the potential to meaningfully improve cardiometabolic health at a broad population level, but the vast majority of eligible U.S. patients have not been prescribed them.
An analysis from the Platform for Evidence GeneraTion in CArdiometabolic HeaLth (PETAL) Study, presented by DCRI’s Nishant Shah, MD, examined the population using these therapies and observed the real-world impact and potential of the GLP-1 RA tirzepatide.
Using electronic health record data from five major U.S. health systems, researchers projected outcomes if 100% of eligible patients were prescribed GLP-1 RAs and took them as prescribed.
“We saw significant reductions in not only patients with diabetes, but also patients without diabetes across weight, hemoglobin a1c, blood pressure, and cholesterol,” Shah said. “But the more striking thing was to see that across patients who are eligible for agents like GLP-1 RAs, under 5 percent of them were even prescribed the medication.
“So that shows that there’s still a critical barrier in the real world to using these medications despite the profound public health benefits that they could have.”
Watch Shah Share Insights From the PETAL Study
Rymer Brings Peripheral Procedure Expertise to AHA Simulation Zone

DCRI faculty member Jennifer Rymer, MD, shared her expertise in peripheral procedures at the AHA Simulation Zone, engaging trainees from around the world through hands-on learning.
Drawing on her extensive experience as a Duke interventional cardiologist, she provided practical insights and guidance.
Rymer worked with participants on a range of peripheral procedures, including renal denervation, iliac intervention, superficial femoral artery occlusion, and lower extremity chronic total occlusion
“We walked through each step and answered questions based on simulated patient scenarios,” Rymer explained. “The goal was to give trainees real-world experience they can take back to their institutions and help them feel confident about techniques. It’s exciting to interact and share knowledge at the AHA.”
Watch Rymer Explain the Simulation Zone
Monday, Nov. 10
Leadless Pacemakers: Transformative Cardiac Care for High-Risk Patients
DCRI faculty member and clinical electrophysiologist Sana Al-Khatib, MD, highlighted best practices for implanting leadless pacemakers, emphasizing indications, key preparation, and procedural techniques.

Leadless pacemakers are small implantable devices that regulate the heart’s rhythm without the need for wires. Al-Khatib called leadless pacemakers transformative to cardiac care for high-risk patients with infection or venous access challenges.
She stressed the importance of ultrasound guidance, heparin administration, and meticulous deployment on the septum to avoid complications such as perforation.
She concluded with a case study illustrating challenges in access and deployment, reinforcing the importance of adherence to safety protocols.
Al-Khatib recommended training for those new to the technology. Seasoned implanters may manage with a local proctor, but dedicated training programs are invaluable for early operators, she said.
The Economic and Clinical Argument for Hospital at Home Care Model for HF

DCRI faculty member Stephen Greene, MD, delivered a compelling analysis of Hospital at Home payment models for worsening heart failure. He provided a background of the care model’s history and current landscape, noting that while hospital care at home may not be the right fit for every patient, more than half of those hospitalized for heart failure could potentially qualify.
He emphasized that, when operating and start-up costs for home-based care are lower than traditional hospitalization, the model makes financial sense.
Clinically, Greene pointed to the opportunity to improve outcomes, citing high readmission rates and limited therapy optimization in conventional care.
“I would argue that the bar is low to improve on the traditional, inpatient care model for worsening heart failure,” he said.
More than half of heart failure patients could qualify for home-based treatment, offering a safer, patient-centered alternative that reduces cost and the patient’s time away from family.
“From a patient-centered perspective, there’s no better way to understand someone’s environment than to care for them in it,” Greene said.